Tagged: Perio-Systemic
Some Remarks on “100 Years of Progress in Periodontal Medicine” (II) – Diabetes Mellitus

ISTOCK/MTHIPSORN under fair use.
That periodontitis and diabetes mellitus are related is known for more than 100 years. While Beck et al. (2019), in their contribution to the JDR Centennial Series on 100 Years of Progress in Periodontal Medicine, start out with a paper by Williams and Mahan (1960), which is mentioned as the first landmark paper (allegedly the first study showing that periodontal therapy reduces insulin requirement; but this study had only shown that removing all teeth with advanced decay improved glycemic control), the latter authors quote a booklet by Otto Georg Grunert of 1899 a patient guidebook for diabetics: Ueber Krankheitserscheinungen in der Mundhöhle beim Diabetes: Therapeutische Winke für Diabetiker. In particular the medical profession had known about the link of diabetes mellitus and oral disease for long.
Further landmark, or “milestone”, papers in Beck et al.’s list on the diabetes-periodontitis relationship appeared around 1996, when late Professor Robert J. Genco, for the first time, had used a slide with the message, Floss or Die! on the occasion of the annual meeting of the American Academy of Periodontology in New Orleans. Some of these studies indeed sparked the idea that it would be possible to reduce HbA1c, the marker of diabetic control, by proper periodontal treatment of diabetic patients.
Some Remarks on “100 Years of Progress in Periodontal Medicine” (I) – Cardiovascular
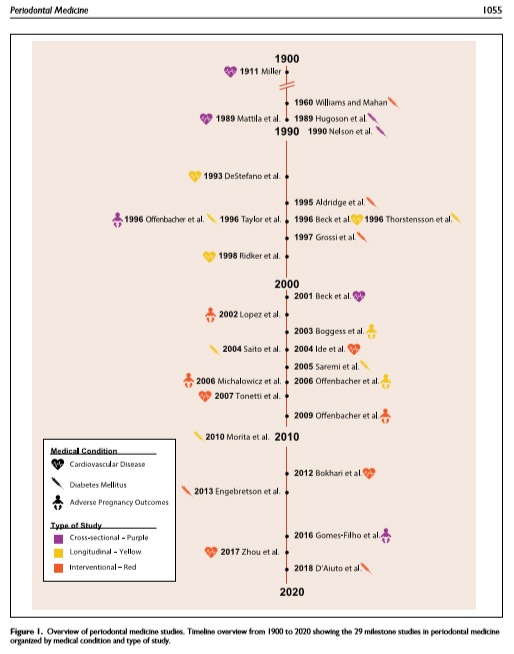
In its “Centennial Series”, an article celebrating Periodontal Medicine appears in next month’s issue in the Journal of Dental Research. The authors James Beck, Panos Papapanou, K.H. Philips and late Steven Offenbacher scrutinize a number of so-called landmark, or “milestone”, studies regarding three pathologic conditions, cardiovascular disease, diabetes mellitus, and adverse pregnancy outcomes. As in every opinion piece, one needs careful reading in order to identify the authors’ bias [1].
Cardiovascular disease
The authors recapitulate the timeline beginning with W.D. Miller’s dental focal hypothesis of 1891. (When writing, I couldn’t get full access to the Lancet article of 1891 to which Beck et al. originally refer.)
They then turn to the stunning (then) observation by Finnish authors Mattila et al. (1989) who adopted a “dental index” of caries, marginal and apical periodontitis, and pericoronitis in a case-control study of hospital admitted patients with recent myocardial infarction and matched controls from official records inhabitants of Helsinki. These authors had set up a logistic regression model adjusted for traditional risks, in particular smoking (former and current smokers) and identified the “dental index” (as well as smoking and, negatively, HDL cholesterol) being statistically significantly associated with myocardial infarction (Odds ratio 1.2586, 95% confidence interval 1.1503; 1.3771, my calculation based on given coefficient and standard error estimates). In two subpopulations, medians of the dental index were 4 and 6. So, the observed odds ratio for increase of 1 score in the index (1.2586) must in fact be considered substantial. This was a single center, low quality (as of current standards) case-control study which had to be confirmed in larger observational and ultimately interventional studies.
Periodontal Therapy For the Management of Cardiovascular Disease in Patients With Chronic Periodontitis

The issue mentioned in the title was dealt with in a systematic review of the Cochrane Collaboration which was published 3 1/2 years ago. It confirmed that, since the publication of the PAVE pilot study in 2009, no further evidence had emerged. The authors of the Cochrane review concluded,
We found very low quality evidence that was insufficient to support or refute whether periodontal therapy can prevent the recurrence of CVD in the long term in patients with chronic periodontitis. No evidence on primary prevention was found.
Possible systemic effects of periodontal treatment had been claimed for a very long time, and lack of evidence, or evidence for their clinical irrelevance, had never been accepted by many colleagues, indeed.
The most recent attempt of reviving the largely lapsed interest by most of our medical colleagues in the Perio-Systemic link, in particular its cardiovascular branch, was launched earlier this week when a delegation of the European Federation of Periodontology (EFP) met colleagues of the World Heart Federation (WHF) in Madrid. The aim of the workshop was to “explore the links between periodontal disease and cardiovascular disease and draw up a series of recommendations.”
Prediabetics, Subgingival Scaling and the Regression Towards the Mean

There is still controversy about the meaningfulness of HbA1c reduction in diabetics upon non-surgical periodontal therapy. One may get the impression that the number of systematic reviews (SR) on the issue surpasses the number of quality randomized clinical trials (RCT). The most current update by the Cochrane Collaboration (Simpson et al. 2015) had concluded that,
There is low quality evidence that the treatment of periodontal disease by SRP [scaling and root planing] does improve glycaemic control in people with diabetes, with a me an percentage reduction in HbA1c of 0.29% at 3-4 months; however, there is insufficient evidence to demonstrate that this is maintained after 4 months.
I will stick to that statement although I am fully aware that attempts are being made by representatives of our profession of considering rather systematic reviews of SRs as if that would lead to other research outcomes. For still interested readers, I have reported and discussed the issue in numerous blog posts, see e.g. here, here and here.
Treating all kinds of systemic ailments by proper scaling and root planing has been an illusion of certain periodontists for some time. As a healthy antidot, one should carefully read an interview with Jan Lindhe, published some time ago, where he warned us:
I think that the dentist’s area is pretty well described – it’s intraoral and also maxillofacial in a sense but the dentist shouldn’t be a pseudo-doctor for all types of disorders. (Emphasis added.)
Scrutinizing the Perio-Systemic Link?
After rather devastating negative conclusions made in a systematic review (SR) of the literature regarding the long claimed, possibly causal, relationship between periodontitis and atherosclerotic vascular disease by Lockhart et al. (2012), a highly alerted group of members of our specialty organizations, the Amercian Academy of Periodontology and the European Federation of Periodontology, had hastily organized a joint workshop, in the end of 2012, to fix unwelcome results of a number of large intervention studies by creating new systematic reviews on the Perio-Systemic link. The clear aim was to cement, once and forever, the claim of the number one clinical problem: periodontal disease and general health are closely related.
While the proceedings had been published, open access, in special issues of our main professional journals, the Journal of Clinical Periodontology and the Journal of Periodontology, workshop participants of the EFP presumptuously condensed the 209 pages of the 16, mostly valuable, papers in a nutshell, strangely called Manifesto.